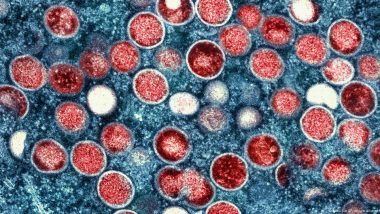
The WHO has declared mpox a global health emergency, the highest level of alert for an infectious disease. DW answers your questions.A new version of the mpox virus has emerged in Central Africa, spreading among children and adults in the Democratic Republic of the Congo and neighboring countries.
Also Read | Unorthodox Cricket Bowling Has Physicists Spinning.
Infection with mpox causes a pus-filled skin rash lasting up to four weeks, which can be very painful.
Also Read | What Does Space Do to an Astronaut’s Body?.
But what symptoms should we look out for and what can we do to reduce the risk of infection?
What is mpox?
Mpox is an infectious disease caused by the monkeypox virus.
The virus was first discovered in 1958 in Denmark, when an outbreak that resembled smallpox was described in monkey colonies kept for research.
Although it is called "monkeypox virus," the original source of the virus is still unknown. Researchers suggest that rodents or small mammals, like squirrels and primates, might harbor the virus.
Mpox cases outside regions like Central and West Africa, where the virus is endemic, have historically been rare and were usually linked to travel or imported animals.
In the span of two years, however, the World Health Organization (WHO) has twice declared the spread of mpox a global health emergency.
In 2022, mpox spread to more than 70 countries that hadn't reported cases previously.
Then, by mid-2024, a new mpox variant had caused a surge of cases and deaths in Congo and in neighboring countries, causing WHO to again declare the spread of the virus an emergency with international concern.
How is mpox treated?
There are no treatments specifically approved for mpox infections (known as "MPXV"). But if you have a strong immune system and don't have a skin disease, you can recover well with appropriate professional care, including pain relief, but without further medical treatment — that's according to the US Centers for Disease Control and Prevention (CDC).
During the 2022 mpox outbreak, a novel antiviral treatment known as tecovirimat was permitted for mpox treatment under a special system, the so-called "Expanded Access-Investigational New Drug" protocol (EA-IND) by US authorities.
Tecovirimat is stockpiled by health bodies for emergency use in the case of a reemergence of smallpox. The WHO declared smallpox eradicated in 1980. But smallpox and mpox are similar in their genetic makeup, so the treatment could be useful. However, the CDC says more data are needed to truly evaluate tecovirimat's effectiveness in treating mpox.
Other treatments under consideration for mpox include brincidofovir and cidofovir. But, as with tecovirimat, the CDC says data are unavailable to fully assess these treatments' effectiveness for mpox.
How does mpox spread?
The virus can enter the body through broken skin, mucous membranes (such as the eyes, mouth and nose) and through the respiratory system.
You can get infected by coming into close contact with people with mpox, such as skin-to-skin contact during kissing, hugging, sex (oral, anal or vaginal) and massages.
Prolonged face-to-face interactions with someone with mpox (like talking or breathing) can cause infection from respiratory droplets carrying the virus.
You can also get mpox from an infected person's body fluids through shared sex toys, bedding or towels. Pregnant people can pass the virus to their baby.
If you are in direct contact with infected animals, you can also contract mpox. This includes skinning, cooking, eating and hunting infected animals or getting bitten or scratched.
An infected person can pass on the virus even before symptoms start, and transmission can continue until all skin lesions are healed and a new layer of skin has formed. This can take weeks.
What are the symptoms of mpox?
The viral infection usually begins with a rash that can be located near the anus or genitals, or on the chest, face or mouth. The rash can then extend to the palms of the hands and soles of the feet and other parts of the body.
The rash can be painful and itchy and resemble pimples or blisters at first, which go through several stages before the scabs fall off.
Flu-like symptoms can start before or after the rash. Those include fever, headache, swollen lymph nodes, muscle aches or chills. Some people report difficulty peeing and a painful swelling of their anus.
Symptoms usually start within 21 days of exposure to the virus.
Dangerous complications can occur when the lesions become infected, leading to abscesses.
Other complications can include severe dehydration caused by diarrhea or vomiting, pneumonia, inflammation of the brain (encephalitis) or the heart (myocarditis) and others.
Who is most at risk?
People who are immunosuppressed because of medical conditions or medication are at higher risk of complications from mpox.
Sex workers, health care workers and people who have multiple sexual partners are at a higher risk of contracting mpox.
According to the CDC, those at risk also include pregnant people, children younger than one, and people with a history of eczema.
During the 2022 outbreak, many people who initially presented symptoms were mainly, but not exclusively, men who have sex with men.
However, the WHO has pointed out that anyone who comes in contact with a person infected with mpox can get infected themselves, regardless of sexual orientation.
How can I prevent getting mpox?
Most people recover from mpox in two to four weeks. If you or your partner has mpox, avoiding having sex, touching or kissing can reduce the risk of spread.
The CDC recommends avoiding close contact with people who have a visible rash at parties, clubs and festivals, where little clothing is worn, and skin-to-skin contact happens often.
Having fewer sexual partners and using condoms also reduces the risk of infection. However, condoms don't prevent infection if you come into contact with lesions or body fluids from other parts of the body.
The CDC has also warned against touching objects handled by a person with mpox, including utensils, towels and bedding, and urged frequent hand-washing.
You can also get vaccinated, although this may not be a current option in your region and might depend on your risk of complications and exposure.
In the US for example, people at high risk of infection or complications can get the Jynneos smallpox vaccine to help prevent mpox.
Because the mpox and smallpox viruses are genetically similar, vaccines that are used to prevent smallpox can also be administered to protect from mpox infections.
Edited by: Martin Kuebler
This article was originally published on August 16, 2024, and updated information on mpox treatment options, August 21, 2024.
Sources:
Amer F, Khalil HES, Elahmady M, et al. Mpox: Risks and approaches to prevention. Journal of Infection and Public Health. Published June 2023.
https://doi.org/10.1016/j.jiph.2023.04.001
Centers for Disease Control and Prevention (CDC). Mpox and Your Health. Published September 13, 2022.
https://www.cdc.gov/poxvirus/mpox/your-health/index.html
Robert Koch Institute, Federal Center for Health Education, Berlin, Cologne. Flyer, transmission and prevention of mpox. Published February 13, 2023.
https://www.rki.de/EN/Content/infections/epidemiology/outbreaks/Monkeypox/Mpox-Flyer_EN.pdf
van Ewijk CE, Miura F, van Rijckevorsel G, et al. Mpox outbreak in the Netherlands, 2022: public health response, characteristics of the first 1,000 cases and protection of the first-generation smallpox vaccine. Eurosurveillance. Published March 2023.
https://doi.org/10.2807/1560-7917.es.2023.28.12.2200772
World Health Organization (WHO). Mpox questions and answers. Published December 11, 2023.
https://www.who.int/news-room/questions-and-answers/item/monkeypox
(The above story first appeared on LatestLY on Aug 21, 2024 03:50 PM IST. For more news and updates on politics, world, sports, entertainment and lifestyle, log on to our website latestly.com).













 Quickly
Quickly