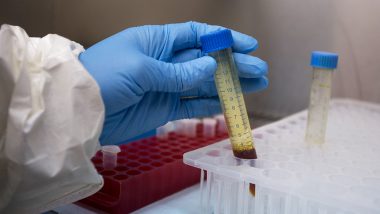
Washington, April 2: Doctor Daniel Brenner has had a busy week in the emergency department of Johns Hopkins Hospital in Baltimore, Maryland, seeing dozens of presumed COVID-19 patients.
As Maryland and other parts of the United States brace for the kind of surges seen in New York and Louisiana, AFP spoke to the fourth-year resident to gain insight into what medical professionals are learning about the disease in real time.
Maryland has thus far seen two dozen deaths and around 2,000 cases -- capacity isn't yet stretched, but could soon be. With hundreds of cases now coming in, Brenner said it becomes "very tricky to tease out who needs to be in the hospital, the people who are at high risk for developing severe symptoms and needing supplemental oxygen" versus those who can recover from home.
Making the right call is crucial, but the problem is compounded by a lack of data to help rationalize choices.
"Is it older people? Is it people with medical conditions?" asked Brenner, adding that doctors were desperately trying to keep up with the latest medical literature as it gets published to stay better informed.
Different physicians have different views, "and there's really no consensus across the country or the medical community which approach is right yet because this disease has only been studied for two months," he said.
The most significant complication for coronavirus patients is Acute Respiratory Distress Syndrome (ARDS) in which the lungs stiffen and become inflamed and the body is starved of oxygen.
Doctors have found placing patients on the stomach in the "prone" position helps prevents fluid from building up in the relatively more healthy area in the back of the lung, said Brenner.
The technique is commonly used on preterm babies requiring ventilators, but for adults it is labor intensive and requires constant monitoring to make sure the breathing tube isn't displaced.
COVID patients also seem to require higher levels of air pressure on their ventilators than people who have developed ARDS by other means, added Brenner.
While hospitals in overwhelmed regions such as New York are in dire lack of personal protective gear, such shortages haven't yet hit other parts of the country. But the virus is forcing medical staff to change the way they work.
In the US, assisted breathing machines called Continuous Positive Airway Pressure (CPAPs) and Bilevel Positive Airway Pressure (BiPAPs) are not being used out of concern that they "might make a giant field of virus" by spraying droplets out of the patient's mouth and nose under pressure, said Brenner.
Ventilators, which place tubes down a patient's air passage, don't have the same problem because the exhaled air is sealed. But this creates its own issues -- BiPAP was typically used for heart failure patients in the emergency room, but now these patients must go on ventilators.
This is a more invasive procedure which requires making them unconscious and giving them drugs to temporarily paralyze the body. In addition to coronavirus cases "we also have everybody else who's critically ill who still has to come to the hospital -- so your heart attacks, your strokes, people who have been hit by a car, those people are still coming," said Brenner.
Their care has to be managed in the context of the virus -- meaning that if a patient comes in with a heart attack and has a cough, they are considered a suspected COVID-19 case. If they are unconcious, they are also presumed positive.
That means donning protective gear even when a heart patient experiences cardiac arrest -- and losing precious time when every second can mean the difference between life and death.
"We all do this because we want to help people, so instinct is 'The patient is in trouble, I have to go in right now, I don't have time to deal with protective equipment,' but we keep telling everyone and keep reminding ourselves that if we get infected we can't help anyone else."
Morale remains high among the medical staff, said Brenner, 36, even as "people are wrapping their heads around the magnitude of this a little bit" and turning to each other for support.
Some staff have been infected at the hospital, but thankfully there haven't yet been any serious cases. One thing that helps, he says, is support from the community in the form of meals sent by local businesses and individuals.
"Sometimes taking a moment and eating a sandwich can make you a much better doctor," he said.
(This is an unedited and auto-generated story from Syndicated News feed, LatestLY Staff may not have modified or edited the content body)













 Quickly
Quickly